Disclaimer: Some of the interview subjects in this story requested not to be named out of fear for their safety and the safety of their properties.
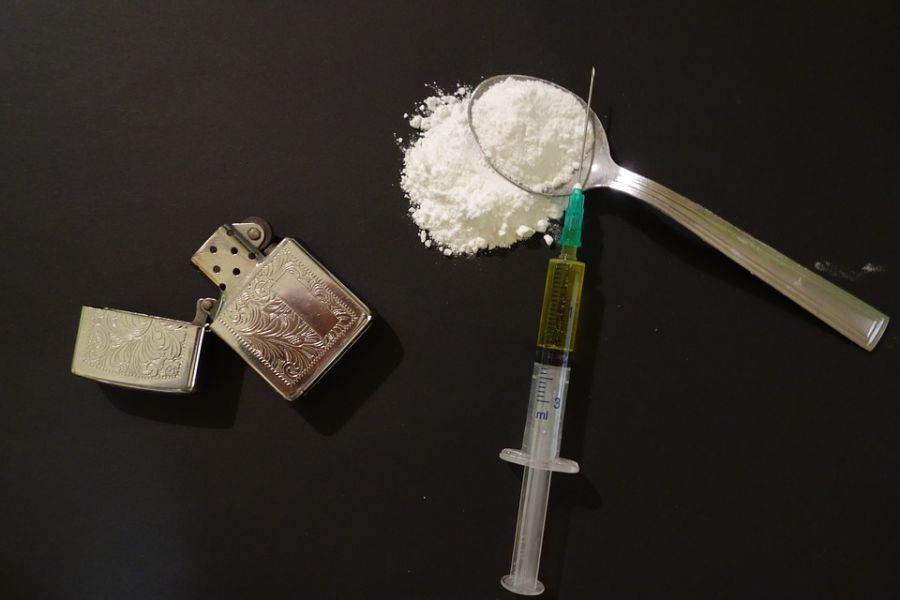
Niagara has a fatal drug problem and Niagara Falls is on top of the list. Residents know it. The mayor knows it. And Ontario knows it.
On Thursday, Ontario Minister of Health Eric Hoskins announced the Ontario government would be providing naloxone, a drug that can revive overdose victims, to police and fire services across the province, as well as asking the federal government to approve and fund safe injection sites province-wide to help combat drastic rises in opioid overdoses
A report by the Ontario government, also released Thursday, said there were 336 opioid-related deaths in Ontario from May to July 2017, representing a 68 per cent increase since 2016.
It said there was a 29 per cent increase in emergency department visits related to opioid overdoses, with 2,449 visits from July to September 2017, compared to 1,896 in the three months prior.
And Niagara Falls sits at the top of those lists.
“It’s embarrassing,” St. Catharines Mayor Walter Sendzik told regional council on Thursday.
“It’s embarrassing because of the fact Niagara Falls is number one, and St. Catharines is number five for statistics that we don’t want to be number one and five at.”
He said himself, Niagara Falls Mayor Jim Diodati and Regional Chair Alan Caslin have been working for a long time to combat the opioid epidemic, but he still doesn’t think enough is being done.
“We can’t keep having committee meetings. People are dying in our neighbourhood,” Sendzik said.
Falls residents who are seeing the drug problem first-hand agree.
Local business owners and residents in the area of Victoria Ave. have said they’ve seen the neighbourhood struggling.
One business owner, who didn’t want his name published, said he knows of three people who have fatally overdosed since July at one address.
Investigation confirmed at least two people did die, and that they had been at the address, though it could not be confirmed where the deaths occurred or if the deaths were caused by overdoses.
Residents of the area say drugs aren’t the only problem either.
With the drugs come other issues like violence, theft and harassment, which are forcing many residents to feel afraid to leave their houses at night.
“I don’t leave the house after dark at all anymore,” said one resident, explaining how she feared being robbed, sexually harassed, assaulted, or worse.
During the summer, at least three people were assaulted (one sexually) while walking on Victoria Ave. at night, according to public police reports alone.
Residents say they want to see serious police response — and quickly.
“It’s not f***ing marijuana,” said one resident who was quite worked up.
“This is clearly a public health emergency and every effort should be made to address this priority issue,” said Niagara Falls Mayor Jim Diodati, in an email sent to council Thursday.
“The province providing naloxone to our first responders is a great first step, but we need to do more — including the establishment of an overdose prevention site,” Diodati said.
But it’s not as simple as just creating a site, explained Valerie Jaeger, medical officer of health for the Niagara Region.
“There has to be an authority to create the space on which a supervised injection site sits, almost as a little piece of not Canada, in the sense that (injecting) is not illegal there,” she said.
Diodati said he will be asking for council’s support at the Dec. 12 council meeting, to “call on the Niagara Region Public Health Department to make opioid addiction response a top priority.”
“We need to build an infrastructure to better diagnose and treat both pain and mental illness.”
Some facts from the Niagara Region:
- There were a total of 155 suspected opioid overdose deaths in 2016. By the end of June 2017, there had already been 209.
- The majority of suspected overdoses occurred in individuals age 26-45, made up of mostly men.
- In 2016, fentanyl was the most common type of opioid present at the time of death, being present in 35 per cent of deaths, followed by hydromorphone, which was present in 25 per cent of deaths.